More than half of Australia’s population over the age of 65 have a cataract in need of repair, equalling more than 70,000 procedures in Australia alone each year. At the Eye and Ear, a junior doctor will learn the process of injecting local anaesthetic via a sharp needle next to eye globe to keep it still and pain free. While usually very safe, complications such as seizures, or blindness may occur in rare cases.
In the last three years, at our hospital alone, six patients have suffered real blindness. Doctors are still reliant on rare and expensive cadavers, ad hoc access to experts, simplistic models, and practice with real patients. There just isn’t enough exposure to rare cases in the training hours available. As part of the continuous improvement at the Eye and Ear, we are enhancing training for doctors, and trainee anesthetists in response to feedback reflecting that 80% of this cohort want access to specialised training.
Practice makes perfect, and simulation of procedural techniques has been proven to increase patient safety and reduces time taken to achieve basic proficiency by more than 50%.
We have created a combined training model with the look, touch, and feel needed for successful practice, in three parts:
- Access to expert knowledge with online e-learning
- Real-world practice via virtual immersive training and life-like anatomical 3D printed simulators or models that provide live feedback for hands-on practice of the procedure (replacing traditional, cadaver tutorials)
- Expert guided workshops for trainees, hosted at the Eye and Ear. Doctors gain expert training, and confidence, patients experience reduced complications and higher satisfaction, and hospitals improve clinical efficiency and reduce risk and cost.
The team has partnerships with world renowned Emeritus professors, anatomists, engineers, clinicians and industry experts from Melbourne, Monash and RMIT Universities and the Eye and Ear. This project has been successful in attracting up to $185,00 in grants in the last two years.
How it works
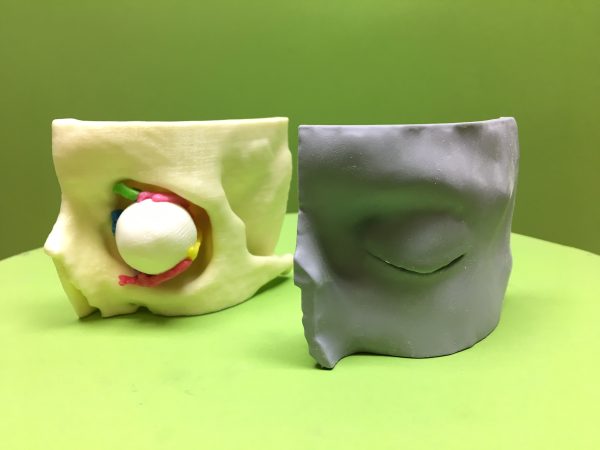
This model will put the ‘flesh’ onto existing 3D printed hard models to bridge the gap in medical education for procedures on soft tissues.
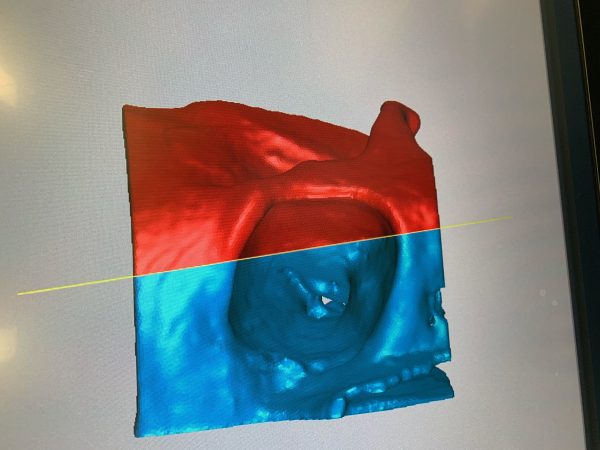
The team has created a disposable orbital cartridge and head for practice, with live feedback and access to rare anatomical differences that you can’t access in the real clinical world. MRI scans are converted to digital files where the specific anatomy is highlighted and coded. This is then converted to files for printing. Materials to replicate the soft and delicate tissues such as skin of eyelids, orbital muscles and the fat between are being created for the first time to replicate real life and in a single anatomically accurate print. It is printed at RMIT with a rare high-tech 3D Stratasys 750 printer, of which there are only three in Australia.
The revolutionary feature of this model is a series of bespoke 3D models of real anatomical pathology with silicone polymers mimicking soft tissue planes and real-time warning, improving patient safety.
We are on track for prototype and e-learning testing, a validation trial and are trialling the first prototype in the coming months. We anticipate multiple models being achieved and that this program will enable much improved patient safety, increased hospital efficiency, and revolutionise medical training.