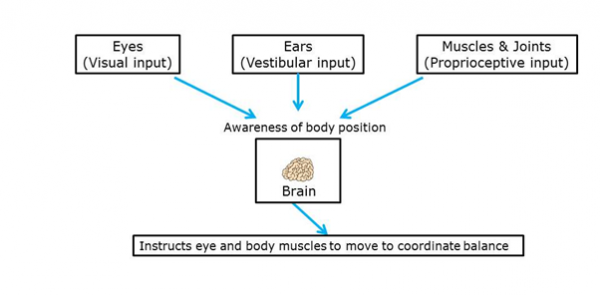
The body’s balance system works through a constant process of position detection, feedback and adjustment. It uses communication between the inner ear, eyes, muscles, joints and the brain.
Key terms
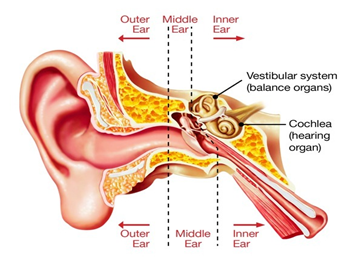
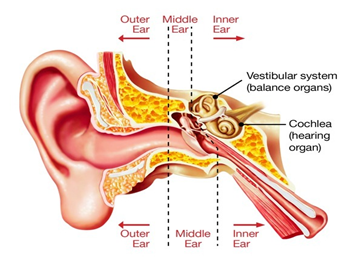
Vestibular system: This is the inner ear balance mechanism. Deep in the inner ears, it sends information to the brain’s movement and balance control centre (the cerebellum) about the position of the head.
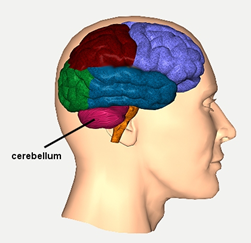
Cerebellum: The brain’s movement and balance control centre.
Otolith organs: Two pockets in the ear’s vestibular system, which together provide constant feedback to the cerebellum about head movement. They are called the saccule and utricle.
Cupula: The internal sensor in the vestibular system that send messages via the vestibular nerve to the cerebellum
Vestibular nerve: Also known as the balance nerve, this is the nerve that send messages from the vestibular system to the cerebellum in the brain.
Visual system: The eyes, muscles and parts of the brain that work together to let us see.
Otoconia: Tiny crystals in the otolith organs in the vestibular system. They shift around with movement to stimulate tiny hairs, which transmit the message via the vestibular, or balance nerve to the cerebellum.
The inner ear is deep inside the ear, just under the brain. One part is called the vestibular system. It is the inner ear balance mechanism. It is designed to send information about the position of the head to the brain’s movement control centre, the cerebellum.
.
The cerebellum is at the back of the head where it meets the spine. It receives messages about the body’s position from the inner ear, eyes, muscles and joints. It then sends messages to the muscles to make any adjustments to posture that are needed to maintain balance. It also coordinates the timing and force of muscle movements that are initiated by other parts of the brain.

Image sourced and used with permission from Centre for Neuro Skills.
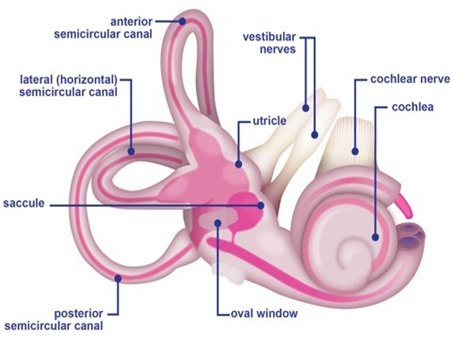
The vestibular system in each inner ear is made up of three semi-circular canals and two pockets, called the otolith organs, which together provide constant feedback to the cerebellum about head movement.

Each semi-circular canal is positioned in a different direction, to detect a variety of movements such as nodding or rotating. Head movements cause fluid inside the canals to move and stimulates the internal sensor (cupula) that send messages via the vestibular nerve to the cerebellum.
The two otolith organs (called the saccule and utricle) send messages to the brain about body movement in a straight line (backwards and forwards or upwards and downwards) and also about where the head is in relation to gravity, such as tilting, leaning or lying down. These organs contain small crystals (otoconia) that are displaced during these movements to stimulate tiny hairs, which transmit the message via the vestibular, or balance nerve to the cerebellum.
The vestibular system works with the visual system (eyes and the muscles and parts of the brain that work together to let us see) to stop objects blurring when the head moves. It also helps us be aware of the position of things, for example, when walking, running or riding in a vehicle.
Sensors in the skin joints and muscles also provide information to the brain on movement, including the position of parts of the body in relation to each other and the position of the body in relation to the environment. Using this feedback, the brain sends messages to instruct muscles to move and make the adjustments to body position that will maintain balance and coordination.